What Chapters of The Arc Need to Know About Managed Care
By Doug Golub, MediSked President and Co-founder
As an increasing number of states transition individuals with intellectual and developmental disabilities (IDD) to managed care, provider agencies are faced with additional complexities to work with Managed Care Organizations (MCOs), including new billing systems, requirements and expectations.
Provider agencies must also ensure that the process of moving to managed care for long term services and supports (LTSS) is based on the principles of self-determination, person-centered planning, and individualized supports. Under the new structure, there are strategies to be utilized to ensure that the benefits available can be translated into a service offering that reflect each individual’s desired outcomes, goals, and lives.
Understanding Managed Care
Managed care is a model of health care delivery that in theory is meant to lower costs and offer budget predictability for states, improve care coordination with providers, and increase quality and outcomes for individuals. Managed care plans are a type of health insurance plan, in which states contract with MCOs and pay a capitated (fixed) payment on a per member per month basis. Capitated Payments can be made on a full or partial basis. “Full capitation” is managed care for all service types (health, welfare, and safety supports) whereas partial capitation may only cover a portion of the Medicaid services offered to individuals.
Under this model, MCOs assume responsibility and accountability for providing coverage of services and improving outcomes for individuals served. Managed care is the predominant delivery system for Medicaid health care services. A large portion of people with IDD rely on Medicaid to live their lives in the community. Some states have made the move to begin including long term services and supports in the managed care system, which they are referred to as Managed Long Term Services and Supports (MLTSS). Several states are using MLTSS to expand home and community based services using different models. Managed care for LTSS is likely to continue to grow.
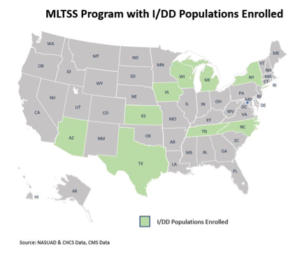
As of June 2017, more than half of all Medicaid beneficiaries (waiver and non-waiver) receive their health care from MCOs. As illustrated in Figure 1,19 states currently operate MLTSS programs, with three additional states operating MLTSS within a Financial Alignment Initiative demonstration.[1] Only nine states (Arizona, Iowa, Kansas, Michigan, New York, North Carolina, Tennessee, Texas, and Wisconsin) have IDD populations enrolled in managed care as they are typically the last group to be integrated into MCOs.[2]
Figures 1 & 2. [MLTSS Programs[3], MLTSS Program with IDD Populations Enrolled, – 2017]

How this Affects Chapters of The Arc
As more states transition to managed care, provider agencies must be aware of how this change will impact them, and be a part of the implementation process at every level from selecting the MCOs to drafting the contracts. Providers must work to:
- Be engaged in the process as states move to enroll individuals with intellectual and developmental disability (IDD) into MCOs
- Prevent the disruption of care
- Examine the benefits available and translate them to service offerings that reflect what individuals they support want and need
| Interoperability 101 |
Interoperability refers to the ability of systems and devices to exchange data. This allows a fuller picture of a person’s health history to improve outcomes, increase transparency and efficiency, and empower individuals. |
Providers are responsible for providing a unique set of services and supports to individuals that must be integrated into the 360-degree view of the individual. A large part of the managed care delivery system requires interoperability throughout the network – agencies must have access to information technology, billing, and systems operations to make the transition to MLTSS.[4]
This required move to electronic health records (EHRs) will allow for more frequent and timely communication between the individual’s network with the ability to share information about demographics, enrollments, authorizations, claims, and assessments. The top priority, however, must be to increase quality of care – and ensure there is no reduction in the quality of supports for the individuals.
Providers will be essential for reporting on health and wellness of the individual and providing quality data reporting by analyzing patterns of service utilization, integrating Quality Assurance measures and functions, and generating quality management reports.
Supporting the Transition
MediSked’s dedicated team of subject matter experts have experience transitioning providers into a managed care model to ensure organizations meet the expectations and have the ability to be technologically sound and compliant. Over 29% of MediSked clients currently bill to MCOs across nine states and the District of Columbia. MediSked is working to provide care coordination and business intelligence tools to MCOs across the country, including Partners Health Plan, the nation’s first Fully Integrated Duals Advantage (FIDA) designed explicitly for individuals with IDD and those that support them.
The Arc of the U.S. and MediSked are committed to making the changes to managed care as seamless as they can be. MediSked is a sponsor of The Arc’s national programs.
“The Arc of North Carolina has been in a managed care system since 2012. A managed care system is all about the numbers – MediSked solutions provide the ability to capture, quantify, and measure data of what is happening and when it’s happening. Technology is essential to gather the empirical data to track what is going on. If you can measure it, you can change it.”
– John Nash, Executive Director of The Arc of North Carolina
[1] National Association of States United for Aging and Disabilities, Center for Health Care Strategies. (2017). Demonstrating the Value of Medicaid MLTSS Programs. Retrieved from: https://www.chcs.org/resource/demonstrating-value-medicaid-managed-long-term-services-supports-programs/
[2] Ibid.
[3] National Association of States United for Aging and Disabilities. (2017). June 2017 MLTSS Map. Retrieved from: https://nasuad.org/initiatives/managed-long-term-services-and-supports/mltss-map
[4] Centers for Medicare & Medicaid Services. (2013). Guidance to States Using 1115 Demonstrations or 1915(b) Waivers for Managed Long Term Services and Supports Programs. Retrieved from: https://www.medicaid.gov/medicaid-chip-program-information/by-topics/delivery-systems/downloads/1115-and-1915b-mltss-guidance.pdf








